“Conflict is a normal part of human interaction. In health care, conflict of some sort has been estimated to occur in the management of a half to two thirds of patients. This conflict most commonly arises between clinicians but also occurs between the clinician and the patient” (Services for Australian Rural and Remote Health, 2013).
In this video, Dr Hayden Richards explores ‘How to address conflict in clinical settings’ (05:27)
Segal and Smith (2013) state that “The ability to successfully resolve conflict depends on your ability to:
- Manage stress quickly while remaining alert and calm
- Control your emotions and behaviour
- Pay attention to the feelings being expressed
Student supervisors require conflict resolution skills, not only for their own practice but also to guide their students through conflict.
Useful resources
- PEP Module 7: Successfully navigating conflicts: This interactive learning module assists supervisors and students to understand conflicts within supervisor-student relationships and to develop strategies to recognise, prevent and manage conflicts.
Identifying student-supervisor conflict in a placement setting
Conflicts between student and supervisor can occur for several reasons and impact on each person’s experience of the clinical placement. Some of these are outlined in the table below:
| Sources of conflict | Examples and explanation | How it might present |
| Expectations |
|
|
| Personality |
|
|
| Supervisory Style |
|
|
| Communication Style |
|
|
| Other |
|
Preventing conflict in placements
“Conflict can be productive when, as a result of listening to other perspectives, a solution is found that may not have been considered previously. It can be destructive when issues are left unresolved or there is coercion and dominance by one group over others" (Services for Australian Rural and Remote Health, 2013).
While it is acknowledged that conflict can be a positive process, supervisors can implement strategies summarised in the table below to minimise negative consequences minimise that may arise if the conflict continues:
| Strategy | Explanation |
| Role model ‘good’ conflict management skills |
Showcase the behaviours that you want your student to demonstrate:
|
| Acknowledge power dynamics |
|
| Managing expectations |
Early in the placements, supervisors need to have an open dialogue to set realistic placement expectations. This might include:
Expectations should be explained as an ‘evolving’ or ‘live’ concept that will be revisited on multiple occasions during the placement. More resources on managing expectations can be found here: Managing expectations, professional boundaries and ethical practice. |
| Institutional planning |
|
Adapted from University of British Colombia (nd), Trinity College Dublin (nd) and McGill University (nd)
Conflict resolution styles
Not everyone approaches conflict in the same way. Supervisors should be aware that the power imbalance that exists in student- supervisor relationships may delay or inhibit their student coming forward to raise issues.
Katz (2007) lists five mechanisms commonly used in conflict resolution and indicates each of these mechanisms may apply depending on the situation. These are illustrated in the table below:
| Mechanism | Application |
| Avoidance | Inconsequential disagreement – staying away from the person or area, hoping it will ‘go away on its own’. |
| Yielding/ Accommodation | Own position is wrong – give in to save problems with ongoing conflict |
| Collaboration | Focus on goals, ‘win win’- work together to identify and implement a solution |
| Compromise | Unable to reach a collaborative agreement – both people give something up to settle the conflict – this results in partial satisfaction for the student and the supervisor |
| Competition | Issue of great importance to each individual, and they can only see it from their perspective. No conciliation possible |
Source: Katz, J (2007)
Tools for dealing with conflict
Conflict’ can sound quite serious, but many ‘conflicts’ are simple misunderstandings that can be resolved. Addressing conflict can often be a source of anxiety or discomfort for both the supervisor and the student.
It is important to address conflict as soon as it arises, to prevent unnecessary escalation and allow the placements to proceed as planned. General principles of providing feedback apply in these instances. A face-to-face meeting should be planned to allow both parties to observe tone of voice and body language.
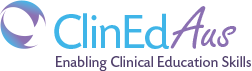
It is worth considering the ‘Positions of Perception’ when addressing a conflict. Supervisors may find the following reflective questions useful when dealing with student-supervisor conflict:
- What am I feeling or doing that may impact on the other person?
- How might the other person feel?
- How might this impact on the team/organisation/client?
Considering the three positions of perception can assist to resolve a conflict by removing the ‘you versus me versus them’. Understanding all positions can lead to a focus on the fourth position of perception, creating a sense of the whole system and how to achieve the goal.
In the meeting with the student:
- Create a positive environment – select a mutually suitable time and scaffold the meeting so that both you/the supervisor and the student understand that the purpose of the meeting is to resolve differences for a mutual benefit
- Establish rules of conduct.
- Allow both parties to bring another person as support (as required)
- Identify the source of the conflict and points of view.
- Find a nonjudgmental starting point for the discussion.
- Establish shared standards and goals.
- Recognise any shared frustrations
- Brainstorm alternatives – what is important to both parties; what are possible solutions
- Problem solve - select an agreed option and determine its implementation plan.
- Display active listening skills
After the meeting, request the student to summarise the discussion that occurred and outline the agreed or next steps. It is recommended that the student supervisor then checks this document to determine the student’s understanding of the situation.
If a conflict escalates, or there is significant issues with student performance and/or behaviour, an external stakeholder (e.g., university placement facilitator) should be invited to a meeting to assist with resolving the issue.
Supervisors should also clearly communicate the counselling or other support that is available for the student should they require it.
In the video below, Julie Gauchwin, Clinical Education Coordinator - Physiotherapy discusses her key strategies for resolving conflict:
References:
Please Note: References remain valid until superseded by later research. The resources referenced here are regularly reviewed and are considered current and relevant to the topics presented.
- Services for Australian Rural and Remote Health (2013).Conflict Resolution. Retrieved from: https://sarrah.org.au/content/conflict-resolution
- Segal, Jeanne and Smith, Melinda (2013). Conflict Resolution Skills. Retrieved from: http://www.helpguide.org/mental/eq8_conflict_resolution.htmGiddings, M., Vodde, R., & Cleveland, P. (2004). Examining Student-Field Instructor Problems in Practicum, The Clinical Supervisor, 22(2), 191-214.
- Katz, Jonathan (2007) Conflict and its resolution in the operating room. Journal of Clinical Anaesthesia, vol 19, pp. 152-158; 2007.
- Giddings, M., Vodde, R. & Cleveland, P. (2004) Examining student-field instructor problems in practicum. The clinical Supervisor 22(2): 191-214 https://doi.org/10.1300/J001v22n02_12
- Hoag, J. (2013). NLP Perceptual positions. Retrieved from NLP Training, coaching, therapy: http://www.nlpls.com/articles/perceptualPositions.php
- University of British Colombia (nd) Module 8 Strategies for resolving conflicts in ‘E-tips for Practice Education’. https://canvas.ubc.ca/courses/97719/pages/module-8
- Trinity College Dublin (nd) Advice for resolving conflicts between supervisors and research students https://www.tcd.ie/graduatestudies/students/research/conflict-resolution/
- McGill University (nd) Supervision – Resolving conflict: https://www.mcgill.ca/gradsupervision/supervisors/resolving-conflict