Providing regular, effective feedback to your student is one of the most important roles of a student supervisor. The opportunities for feedback during a placement include:
- Informal feedback: information communicated to the learner as part of the normal day-to-day interaction.
- ‘Formative’ feedback: information communicated to the learner that is intended to modify his or her thinking or behaviour for the purpose of improving learning.
- Formal 'summative' feedback: information communicated to the learner that is associated with assessment.
On this page you will find:
(Click on the accordion titles below to explore the content areas)
-
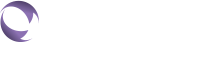
Preparing for a feedback session
Preparing for a feedback session
Before you provide feedback, it is important to consider your expectations and share these with the student. Preparing for a feedback session should involve:
You may find it useful to consider the evidence on feedback models and methods to assist you in preparing and planning your feedback session.
-
Giving quality feedback
Giving quality feedback
Quality feedback needs to be:
- Focused on patient centred care
- Timely and in an appropriate setting
- Objective, specific, constructive, and balanced.
This next video explores these elements in more detail:
A feedback session that incorporates the components identified in the video above, should be a dialogue between two people, i.e., you (the supervisor) and the student:
- Encourage two-way discussion through use of active listening and elements of advanced questioning.
- Remember to be aware of you and your student’s body language and moderate how fast you’re talk during the session.
- Use pauses to allow the student to consider the feedback and seek clarification if they require.
- Provide students with an opportunity to comment on the feedback and to provide explanations for their performance. It is important to remember that students may not be used to receiving feedback or their previous experience of feedback may have been poor. Be prepared for an emotional response from the student, and encourage them to take a break if required.
- Monitor for understanding. Allow time and provide opportunity for the student to react, reflect and respond. This might be by including statements or questions like: “Let’s decide together on the action plan required to address the feedback".
Asking the student for feedback on the supervision provided can also be good role modelling. This can assist to promote a work culture where ‘feedback’ is the norm. It also aids in the development of the student-supervisor relationships, and it may identify ways in which you can improve your supervisory skills. It can also reduce a perceived power imbalance if you, the supervisor, reveals your own vulnerabilities and acknowledging that your learning is ongoing.
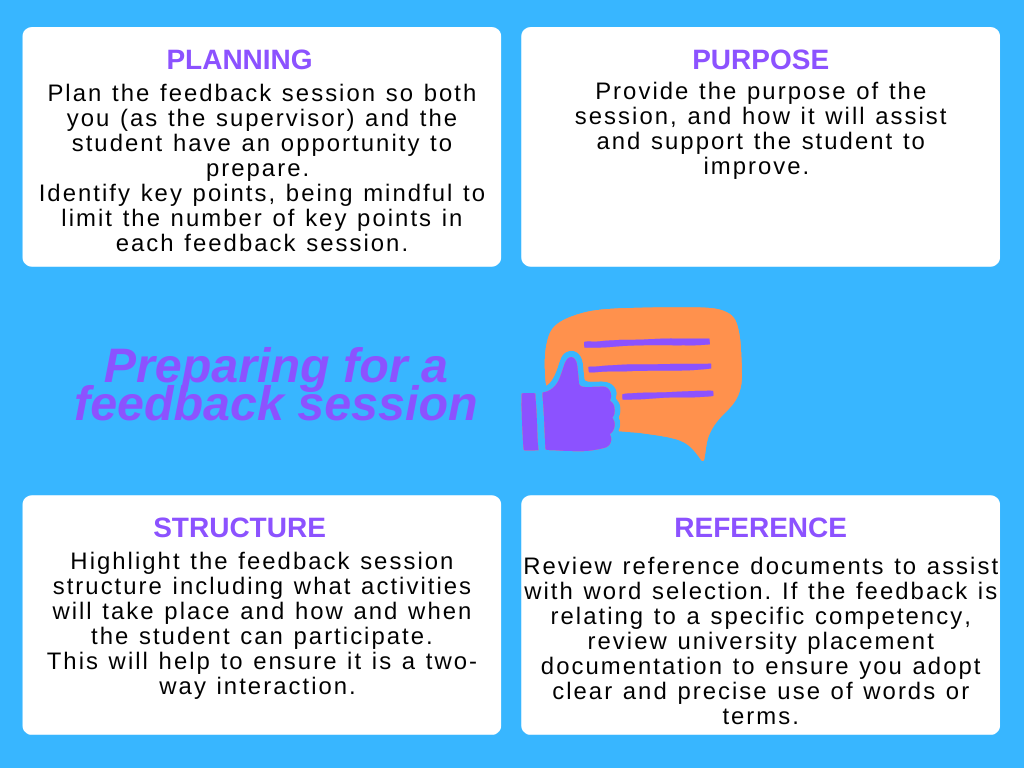
In the figure below, Weallans and colleagues (2021) explore the sequential process of providing feedback:
-
Barriers to effective feedback
Barriers to effective feedback
There are many barriers to providing effective feedback, including:
- Lack of supervisor confidence in the delivery of feedback and fear of upsetting the student can affect the student supervisor relationship and be a barrier to the delivery of effective feedback
- Language and cultural differences that affect the way feedback is given and received can also be a barrier to effective feedback if not managed appropriately.
- Not having sufficient time to provide constructive feedback
- Feedback that is considered a criticism rather than being constructive
In this video, Dr Hayden Richards discusses how to seek constructive feedback (05:55)
-
Video Scenarios: Ineffective and Effective Feedback
Video Scenarios: Ineffective and Effective Feedback
These four scenarios explore the impact of communication skills on feedback to a student on placement.
In scenario 1 the student supervisor provides the student with his view of the session. The feedback is clear and specific but not constructive. The student supervisor does not acknowledge what the student has done well. He does not use positive body language and fails to interpret the student's body language while giving feedback. In scenario 2 the student supervisor's message is not clear and the student is left wondering about the key take home messages including how to improve their performance.
In scenario 3 the student supervisor is positive about the student's performance, but time poor. In the final scenario, the student supervisor has well-developed and effective communication skills. The feedback process facilitated a discussion where the student is engaged and reflects on her performance. -
Useful resources
Useful resources
Fact sheets and guides
- GUIDE - University of Adelaide - Active Listening Learning Guide - Active listening is a skill that greatly enhances the efficacy of feedback, reflective practice and facilitation of clinical reasoning. It demands alertness on the part of the listener (Trevithick, 2000 as cited in Health Education & Training Institute, 2012), aiming to understand the intended message as well as the content.
- FACT SHEET - Framing Feedback
- FACT SHEET - Briefing and Debriefing - Briefing and debriefing can be simple interactions between the supervisor and student and can have long lasting effects on how the student placement unfolds. The purpose of briefing is to optimise student learning by addressing student expectations and feelings about new and unfamiliar
- VIDEO - This video ‘Briefing and debriefing’ (02:12), presents tips for briefing and debriefing in a mental health care setting .
ELearning professional development
- Supporting Health students in the workforce Tasmanian Clinical Supervision Learning Package for Health Professionals has been developed to help guide and support clinical education and supervisor training activities in Tasmania. The 4th module in the series of open access eLearning modules is on ‘Constructive feedback’
- PEP Module 6: Feedback and evaluation: This interactive learning module provides supervisors and students with practical tips and strategies to ensure feedback and evaluation are a positive and rewarding experience.
- University of Sydney - Effective feedback learning module
-
References - Providing feedback
References:
Please Note: References remain valid until superseded by later research. The resources referenced here are regularly reviewed and are considered current and relevant to the topics presented.
- ACT Government, (nd) ACTPS Performance Framework: The Art of Feedback: Giving, seeking and receiving feedback. Accessed November 2020 from https://www.cmtedd.act.gov.au/__data/assets/pdf_file/0003/463728/art_feedback.pdf
- Duffy, K., (03.04.2013). "Providing constructive feedback to students during mentoring". Nursing standard (0029-6570), 27 (31), p. 50.
- Hardavella, G., Aamli-Gaagnat, A., Saad, N., Rousalova, I., & Sreter, K. B. (2017). How to give and receive feedback effectively. Breathe (Sheffield, England), 13(4), 327–333. https://doi.org/10.1183/20734735.009917
- Health Education and Training Institute (2023). Clinical supervision: The superguide: a handbook for supervising allied health professionals https://www.heti.nsw.gov.au/education-and-training/our-focus-areas/allied-health/clinical-supervision
- Health Education and Training Institute (2023). Clinical supervision: The Learning Guide a handbook for allied health professionals facilitating learning in the workplace. https://www.heti.nsw.gov.au/education-and-training/our-focus-areas/allied-health/clinical-supervision.
- Health Workforce Australia (2013). Enabling Clinical Supervision Skills. Griffith University, Gold Coast.
- Johnson CE, Keating JL, Molloy EK. Psychological safety in feedback: What does it look like and how can educators work with learners to foster it?. Med Educ. 2020;54:559-570. https://doi.org/10.1111/medu.14154
- Weallans J, Roberts C, Hamilton S, Parker S. Guidance for providing effective feedback in clinical supervision in postgraduate medical education: a systematic review. Postgrad Med J. 2021 Feb 9:postgradmedj-2020-139566. doi: 10.1136/postgradmedj-2020-139566. Epub ahead of print. PMID: 33563716.